Vial / Ampoule Swaps
Overview
While there are many opportunities for anesthesia providers to make a medication error in the perioperative area, selecting a drug container from which a medication dose must be withdrawn is one that makes these caring professionals especially vulnerable. The anesthesia provider could accidentally pick up the wrong vial or ampoule, especially if it looks similar to another container, if it is placed near another similar looking medication on the anesthesia cart or the OR prep table, or if it is improperly stocked in the anesthesia cart. In fact, vial and ampoule swaps are among the top three most common medication errors made in the operating room.
Customer experience:
“Pharmacy improperly stocked a 10ml vial of Phenylephrine in the anesthesia cart where Neostigmine should have been – look alike drugs that can be easily confused. The anesthetist pulled what he thought was Neostigmine then scanned it on SLS. The visual and audible safety checks alerted him that the drug was not in the formulary so he took a closer look, then realized he had the wrong drug. Had the incorrect medication been administered, the patient’s blood pressure would have spiked and, although every patient is different, something much worse was possible.”
—Jason St. Amour, Pharmacy Operations Manager, South Shore Hospital
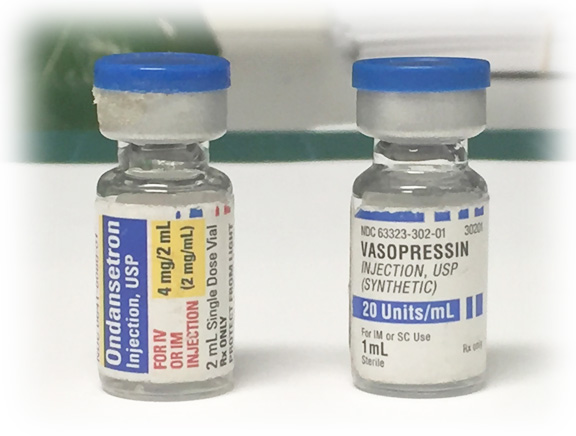
Look-Alike / Sound-Alike Medications:
Elements of Performance for MM.01.02.01
1. The organization develops a list of look-alike/sound-alike medications it stores, dispenses or administers
(https://www.ismp.org/tools/confuseddrugnames.pdf)
How Safe Label System helps hospitals meet the standard:
When a clinician scans a vial/ampoule on SLS, an immediate visual and audible confirmation identifies the drug in hand, acting as a second set of eyes. This safety “double-check” helps ensure that the medication selected is indeed the medication the clinician intended to select. On demand, SLS produces a 100% TJC-compliant label that is ready to apply to a syringe. These labels comply with ISMP/FDA Tallman lettering recommendations as well as ASA, USP, ASTM, ISO, ISMP and APSF standards.
2. The organization takes action to prevent errors involving the interchange of the medications on its list of look-alike/sound-alike medications.
How Safe Label System helps hospitals meet the standard:
SLS is based on a drug formulary, managed by pharmacy, that uniquely ensures compliance with best practices and hospital policy. It consolidates TJC, USP and ASA guidelines, coupled with pharmacy-guided formulation, to be available anywhere medications are prepared to improve patient safety, efficiency and accuracy to reduce medication errors.
In 2010, the APSF proposed a paradigm to reduce medication errors causing harm to patients in the surgical suite – STPC: standardization, technology, pharmacy/prefilled/premixed and culture. Specifically, in their technology review, APSF made recommendations that can address the human errors aspect of vial/ampoule swaps:
- Employ a barcode scanning system to identify medications before preparing and/or administering them (Eichhorn, 2010)
- Provide a standardized, machine-readable barcoded label on all drug containers and/or syringes dispensed to the perioperative setting, or employ a similar just-in-time labeling system that can be used in the surgical setting (Eichhorn, 2010)
- Employ an electronic mechanism to provide feedback, decision support, and documentation of important data during the perioperative encounter (Eichhorn, 2010)
- Provide large and loud visual and auditory stimuli targeting multiple senses to verify drugs and concentrations, and to communicate important alerts.
Safe Label System technology answers the call of the NPSG and APSF. SLS safeguards the patient against vial/ampoule swaps and, in doing so, has a profound affect for the patient. SLS delivers the necessary safety checks that act as a second set of eyes at the point of care achieving an unparalleled improvement to healthcare quality.
